Posting a Medicare Sequestration Payment
Sequestration is the term that applies to the 2% payment reduction to providers that became effective for dates of service April 1, 2013 and after. This policy is required by The Budget Control Act of 2011. It requires, among other things, mandatory across-the-board reductions in federal spending. The claims payment adjustment shall be applied to all claims after determining coinsurance, any applicable deductible, and any applicable Medicare secondary payment adjustments.
For more information about the legislation in general, check out:
American Medical Association FAQ
Important to Remember
The 2 important concepts to remember is to reduce the allowable but keep the contractual discount the same.
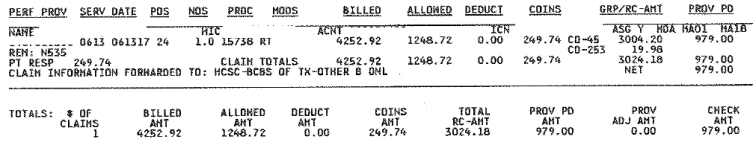
Review the Medicare EOB (Explanation of Benefits)
Important Numbers
Billed - should be the amount you charged.
Allowed - the maximum amount that an insurance plan will consider to pay for a service, including any amount that the patient will be responsible for paying. If you are In-Network, the allowed charge is based on your contract with the health plan, and you cannot collect more than that amount. If you are Out-of-Network , this is the Usual and Customary amount, but you can collect more than the allowable because you are not bound by a contract.
Deduct - patient responsibility; in some situations, this is billed to the Secondary Insurance Plan. Currently, the Part B (Outpatient) deductible is $183 per year.
Coins - patient responsibility; in some situations, this is billed to the Secondary Insurance Plan. This is currently 20% of allowed.
GRP/RC-AMT - contains the type of assignment (ASG). A "Y" indicator shows the provider accepted assignment. A "N" indicator shows a non-assigned claim. Under the assignment indicator are the non-covered service amounts. These amounts will equal the difference between the billed amount and allowed amount. The last field in this column is a total of the non-covered amounts. Two important indicators are:
- CO-45 - Exceeds the Contracted Fee. This is the difference between the amount you billed and the allowed amount.
- CO-253 - Sequestration - Reduction in Federal Payment. This amount basically reduces the Allowed amount, so you cannot collect that money from the patient.
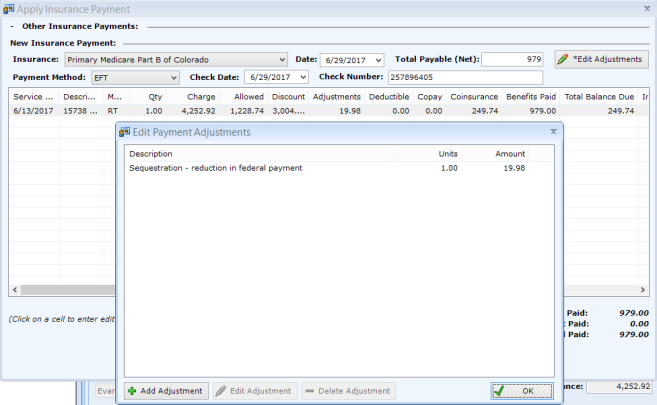
Post the Payment in patientNOW
Allowed - Allowed Amount - Sequestration ($1,248.72 - $19.98 = $1,228.74)
Discount - CO-45 Amount ($3,004.20)
Adjustment - (double-click in Adjustment column to display Edit Payment Adjustments dialog) - CO-253 Amount ($19.98)
Coinsurance - COINS Amount ($249.74)